; ?>/images/banner.jpg)
Some animals are nocturnal by nature, that is, they are most active at night, such as opossums and raccoons. Other animal like humans, are diurnal by nature, that is, they are most active during the day. Like the wolf ancestors that they descended from, dogs are neither nocturnal nor diurnal, but crepuscular.
Crepuscular animals are most active in twilight, which is the periods of the day around dusk and dawn. Also like wolves, to accommodate their lower light preference, they have even evolved a special reflective region of the retina that enhances vision in a lower light setting. This is why the eyes of wolves and dogs can seem to glow in low light when just small amounts of light reflect off the eyes.
Dogs can be incredibly adaptable and can seem to conform to human preferences in many aspects of life, including the periods when we tend to be most active. And while it is a dog’s general preference to be the most active in during the twilight periods of the day, it is not necessarily bad for the dog to be active alongside their humans when we generally choose to be the most active. However, it is wise to always be cognizant of the dog’s innate preference for a crepuscular existence and at least try to meet them part of the way.
From a training perspective, a dog is going to be the most alert, mentally acute, and receptive to learning during the twilight periods of the day. Therefore, you should aim to plan training sessions around dawn or dusk. This will enable your dog to get the most out of training sessions and optimally learn.
While for many of us, dawn is a bit on the early side to get up and walk our dogs and play with them, but you should not too much time elapse from dawn to start engaging with your dog. By their nature, they crave to be most active when the sun is lower, so a good compromise is to be certain let them out and engage with them no later than 60 to 90 minutes after dawn. While it will be brighter than sunrise, the sun will still be lower in the sky and your dog will far more relish play than he would with the sun much higher in the sky and brighter later in the day.
On the flip side, don’t try to keep your dog active late into the evening, as the dog’s mind and body are seeking rest and winding down the farther they get from dusk. At the same time, it is good policy to let them out to potty late enough that they will not have to go in the middle of the night, so a good rule of thumb is to have their final walk and potty outside 60 to 90 minutes after dusk.
Dr. Roger Welton is a practicing veterinarian and highly regarded media personality through a number of topics and platforms. He is the author of his top selling memoir The Man In The White Coat: A Veterinarian’s Tail Of Love. In addition to this writing this blog, Dr. Welton also hosts the popular Space Coast Pet Podcast. He is the CEO and chief attending veterinary of Premier Veterinary Care in Viera, FL.
It has always been astounding to me the number of pet owners who decline stool parasite screening as a regular component of the well visit. Statistically I have found that 48 percent of pet owners decline yearly parasite screening despite my assertions that these parasites can be monsters within that not only chip away at the health of the actual patient but could put the human family at risk as well. From a medical perspective , routine parasite screening has always been an essential component to maintaining the health of the animal patient and the human family he resides with . However, now with the emergence of resistant parasites, routine parasite screening has never been more important.
What we refer to using the term “resistant parasite” , is the emergence of parasites that are no longer eradicated using our traditional anti-parasite medications. That is, they have gained genetic resistance to the effectiveness of parasite medications that have previously been effective in treating parasites for years.
Particularly concerning are resistant strains of hookworm that we have been encountering starting here in my home state of Florida, but now spreading throughout the southeastern United States; and it is predicted that eventually those strains will be nationwide. In light of the emergence of these resistant hookworm strain, we find ourselves having to get creative with anti-parasitic cocktails in order to successfully treat them. There is even a strain that infects primarily greyhounds for which there is actually no effective treatment.
So why should pet owners be concerned about this? Hookworm is well-documented to chip away at the health of the Patient either with direct irritation of the bowel and malabsorptive syndrome , but when subclinical (meaning no direct GI symptoms), is known to chip away at the health of the patient by zapping its nutrients and reducing the effectiveness of his immune system. On the human side, hookworm can infect a person and reach a larval stage that can migrate through the skin and cause severe itchiness, discomfort and cause spider web looking lesions on the skin. These type of larvae are called cutaneous larval migrans. I have a family member who contracted this from his puppy that was infected with hookworm and it took several rounds of medication and weeks of discomfort to rid himself of the parasite.
There is also an emergence of resistant strains of giardia, a protozoal parasite that also primarily infects the gut. While giardia remains species specific and the canine and feline versions do not appear to currently have the ability to infect people, the ability for an organism to jump species often starts with the emergence of strains resistant to medication that would normally successfully treat them.
Thankfully, we have new technology at our disposal to not only highly accurately identify the presence of parasites , but can also identify resistant strains. Traditionally, most stool tests relied on a technique where ultimately the main diagnosis is obtained by a technician literally looking under a microscope and looking for eggs produced by certain worm parasites and cysts produced by certain protozoal parasites. These tests had uncomfortably high rates of false negative as high as 25%, but also did not enable us to identify specific strains of parasites. This still served us pretty well given that resistant strains of parasite are only a recent phenomenon, but now knowing that they are among us it is important to know if we are dealing with a resistant strain right out of the gate.
Specifically, instead of relying on the human element of visually searching for parasite components, we now have gastrointestinal PCR testing at our disposal that takes a human element out of the testing and makes it highly accurate. PCR identifies DNA signatures from the individual parasites present in the stool and not only finds the organism but tells us the exact strains so that we know if a patient is infected with a resistant strain; and can therefore get aggressive with the treatment immediately . It costs a bit more than traditional stool parasite screening, but in my opinion given the potential health benefits of catching these parasites strains before they wreak havoc on the health of the patient or put the human family at risk , are priceless.
I recommend that the next time your pet has a yearly well visit , ask your vet about GI PCR parasite testing instead of traditional diagnostic techniques. For a slight uptick in cost you will receive a high level of diagnostic accuracy never-before-seen and if positive, be armed with knowing the exact strain of parasite and therefore the best way to treat it.
Dr. Roger Welton is a practicing veterinarian and highly regarded media personality through a number of topics and platforms. He is the author of The Man In The White Coat: A Veterinarian’s Tail Of Love. In addition to being passionate about integrative veterinary medicine for which he is a globally recognized expert, Dr. Welton was also an accomplished college lacrosse player and remains to this day very involved in the sport. He is president of Maybeck Animal Hospital , general partner of Grant Animal Clinic, and runs the successful veterinary/animal health blogs Web-DVM and Dr. Roger’s Holistic Veterinary Care. Dr. Welton fulfills his passion for lacrosse through his lacrosse and sport blog, The Creator’s Game.
The cranial cruciate ligament (CCL) is the major stabilizing ligament that lies deep within the knee joint in dogs and serves a similar function as the anterior cruciate ligament (ACL) in people. Rupture or tear of this ligament is a very common injury in the hind extremities of dogs. Rupture of the CCL causes a forward thrust, also known as a sheer force, of the tibia when the dog is in motion or even just standing while weight bearing. The image below illustrates the nature and consequence of rupture of the CCL.
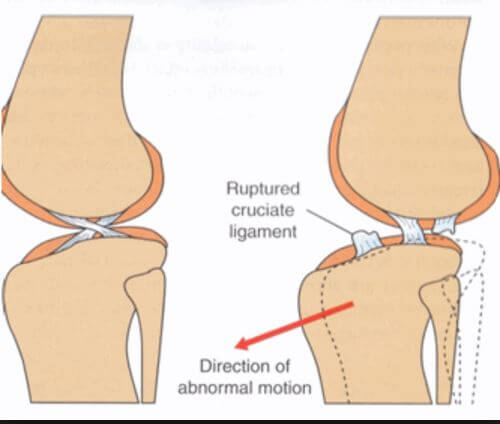
The sheer force causes inflammation and pain within the joint and causes significant lameness in the affected limb. CCL rupture will not heal without surgical stabilization. The longer a dog lives with a CCL tear, constantly shifting weight to the non-injured limb, it increases the chance of CCL tear in the opposite limb.
There are three main methods by which dog knees with torn CCL’s are surgically stabilized. One approach involves running a suture between focal points of the femur and tibia. Suture procedures still have their place in CCL repair, but it is widely accepted that suture based CCL repair is not as effective for dogs over 35-38 pounds. My own preference for suture procedure for surgical stabilization is the arthrex tighrope suture procedure for CCL tears in smaller dogs generally south of 35 pounds.

Larger breed dogs will tend to place a great deal of force across the knee joint that sometimes leads to suture failure. Also, certain large breed dogs are born with steep tibial head angles (called tibial slope – more on this below) that predispose the dog to the injury in the first place, that will subsequently fight against the suture for the life of the dog. Thus, procedures called osteotomies are generally the preferred method of repairing CCL injuries in large breed dogs. Osteotomy refers to procedures that require the cutting and altering of long bone structures.
In the 1990’s, a procedure was developed by an Oregon based veterinarian called the tibial plateau leveling osteotomy, aka, TPLO. The procedure involves cutting a wedge of bone out of the head of the tibia, rotating it a predetermined number of degrees, and plating in place. This changes the physics of the knee by altering the angle of the surface of the head of the tibia (aka, tibial plateau), whereby the sheer force created by the injury is converted into a compressive force oriented toward the vertical axis of the femur. The resulting compressive force is not painful for the dog and successfully stabilizes the knee when the dog is weight bearing or in motion (stay tuned for more on the compressive force, as this is an important consideration). The subsequent reduction of the tibial slope accomplished by the TPLO also accounts for the aforementioned certain breeds that have steep tibial slope angles that predispose to CCL injury. The x-rays below show pre and post operative TPLO images.
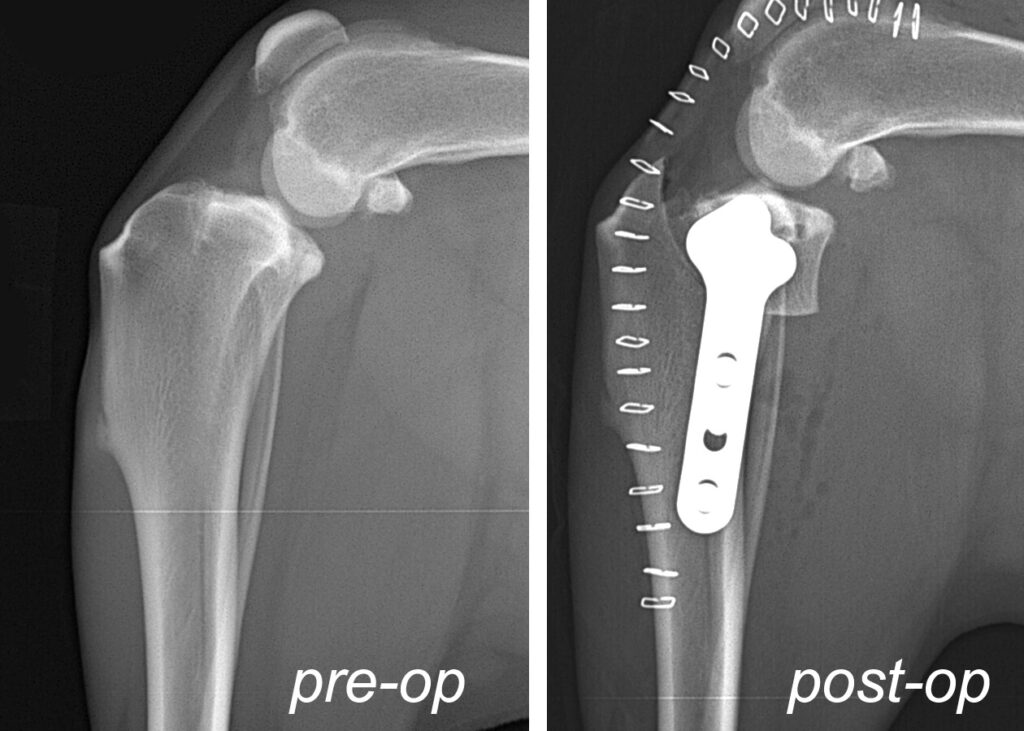
Although the procedure was invented in the United States, TPLO at first gained more momentum in Europe as the procedure of choice for CCL tear in medium to large breed dogs. It started to gain momentum in the US in the early 2000’s and has generally currently become the CCL repair method of choice among veterinary colleges and the majority of veterinary surgeons. Many even hold it as the procedure of choice even for small and toy breed dogs. But hold that thought, there is much more to come!
In 2005, a procedure known as the Tibial Tuberosity Advancement (TTA) was developed in Switzerland where the top part of the tibia, called the tibial tuberosity, is cut and advanced forward. The result is two fold:
1.) The advancement increases tension on the very thick and strong patellar tendon that runs over the knee cap and inserts at the head of the tibia. This increased tension on the patellar tendon stops the sheer force created by the CCL tear.
2.) The advancement of the tibial tuberosity lengthens the patellar tendon thereby decreasing its angle relative to the tibial slope (the portion of the tibia that articulates with the femur within the knee joint). The result is that the deep tibial slope angles are to some degree functionally reduced without the necessarily having to change the angle by cutting such a large wedge of bone as is the case with TPLO. Overall, TTA was considered by many veterinary surgeons to be less invasive and found that patients were quicker to weight bearing and experienced less complications. What’s more, the procedure had a shorter learning curve than TPLO, so veterinarians without residency training were able to quickly gain proficiency with the procedure.
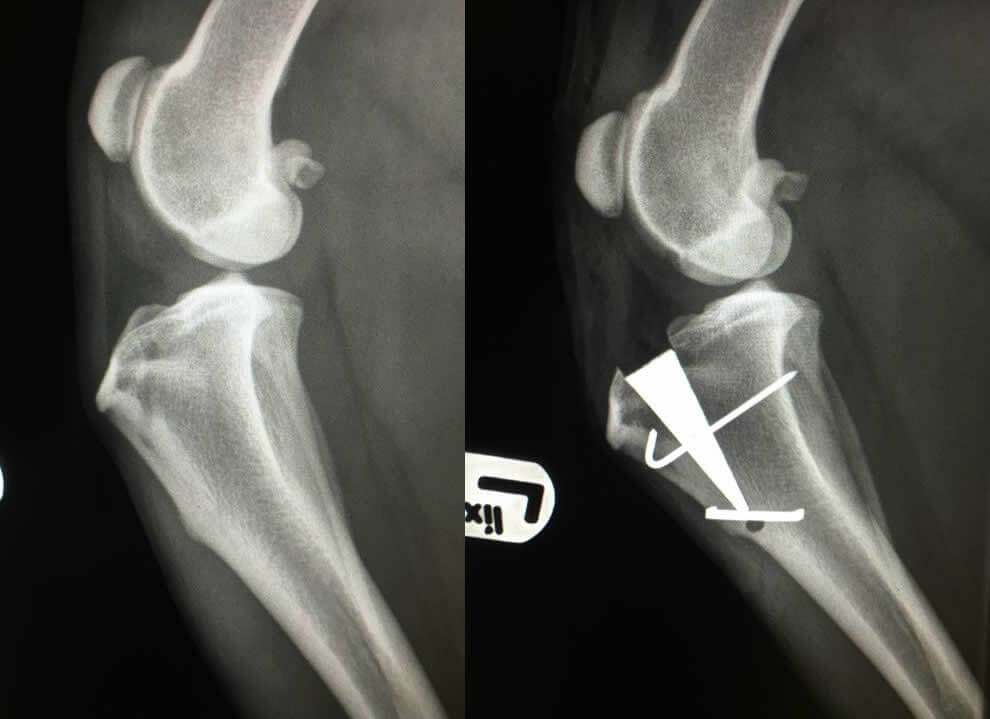
Below is the post operative TTA x-ray:

I am not really certain why veterinary colleges never really embraced the TTA as a mainstream CCL repair procedure performed at veterinary college teaching hospitals. Despite the European veterinary community making a significant transition away from TPLO to TTA after its inception in 2005, while many private US veterinary surgeons were adopting TTA as their go to procedure, US based veterinary schools stuck with TPLO.
Enter the Modified Maquet Procedure, aka, MMP, developed in England and first introduced in the US in 2014. The MMP procedure utilizes the same principles as the TTA, however, with less cumbersome hardware, smaller incision, and shorter surgical time. The wedge that is placed within the bone does not require multiple screws to be placed into the bone as the TTA and TPLO hardware does. Once placed, it simply requires the placement of one single pin and staple that effectively hold the hardware in place. What’s more, the MMP wedge is made of a porous titanium alloy that allows bone to grow through it. This results in much faster recovery times of 4-6 weeks (as opposed to TPLO and TTA that are 10-12 weeks). See the images below for a post operative MMP x-ray and an image of the actual hardware used in the procedure:

Let’s return to TPLO for one moment before I close. Remember I wrote about converting the sheer force into a compressive force? No, it is not painful and, yes, it stabilizes the knee, but it is not without consequence. Over time that compressive force leads to earlier stage degenerative joint disease of knees surgically repaired via TPLO as compared to TTA and MMP; in my experience in dealing with degenerative joint issues in dogs’ senior years that have had past CCL surgical repair. Also, look back at the TPLO x-ray and observe the metal structures across the surface of the leg….those are skin staples necessary to close the skin and give you an idea of the size of the incision. That represents an 8-10 inch incision versus MMP that requires typically no more than a 3-4 inch incision.
This is not to say that TPLO does not necessarily have its place in some cases. Before deciding on which procedure to move forward with, it is imperative to measure the tibial slope angle. The reason for this is that occasionally, dogs that suffer CCL tear have done so due to an inherrited excessively steep tibial slope angle that causes excessive forward thrust of the tibia and stresses the CCL. While the MMP functionally overcomes many cases of excessively steep tibial slope, I generally will not recommend MMP for patients with tibial slopes of 28 degrees or higher. Dogs with slopes above this threshold should have TPLO done, as it more aggressively addresses reduction of the tibial slope angle. Luckily, tibial slopes of 28 degrees or higher has only represented a very small percentage of my cases, so MMP remains the appropriate surgical repair for the vast majority of my patients that present with CCL tear.
I am enjoying quicker return to function, by far faster recovery times, and excellent results with the MMP procedure for repair of the CCL in dogs that I have been performing the surgery for since completing the training in 2017. The standard TTA and TPLO remain good procedures especially in the hands of an experienced veterinary surgeon, but in my view, MMP is currently the best CCL repair procedure for most dogs over 38 pounds that have suffered CCL tears.
Related: The benefits of Modified Machet Procedure (MMP) over TPLO surgery for CCL tears in dogs
Dr. Roger Welton is a practicing veterinarian and highly regarded media personality through a number of topics and platforms. He is the author of The Man In The White Coat: A Veterinarian’s Tail Of Love. Dr. Welton is the CEO and senior attending veterinarian of Premier Veterinary Care in Viera, Florida. In addition to blogging, he is also the host of the popular Space Coast Pet Podcast.

Dog have a long established history of being able to detect health conditions in people. There are service dogs that are trained to predict or recognize seizures in epileptics to assist in protection and alert. There are dogs that can sniff out cancers of the skin and and internal cancers that result in a change of smell in the urine or blood. There are even dogs that can sniff high or low blood glucose levels to alert diabetics. Is it possible that our canine companions with superhero olfactory senses can be trained to sniff out novel coronavirus?
The University of Pennsylvania School of Veterinary Medicine is trying to find out just that with a new program to see if dogs can detect the current strain of the coronavirus, aka, COVID19. The program is currently training dogs to learn how to identify different smells, beginning with sniffing out an odor successfully to be rewarded with a treat. After a successful first training period, the dogs will then begin to use samples from patients who have tested both positive and negative for COVID-19.
The program aims to identify if there an odor associated with a volatile organic compound associated with COVID-19 and see if the dogs can sniff out the difference. The hope is that the doctors at Penn can successfully then train the dogs to help sniff out the COVID-19 in infected people.
Per the program’s director, Dr. Cynthia Otto, if testing and training is successful, it would not be a replacement for standard COVID-19 testing. She views it as ancillary and complementary, such in scenarios like having employees walk by the dogs as they enter the workplace and the dog would alert if someone was positive.
Primary source for the article was https://abcnews.go.com/
Dr. Roger Welton is a practicing veterinarian and highly regarded media personality through a number of topics and platforms. He is the author of The Man In The White Coat: A Veterinarian’s Tail Of Love. In addition to being passionate about integrative veterinary medicine for which he is a globally recognized expert, Dr. Welton was also an accomplished college lacrosse player and remains to this day very involved in the sport. He is president of Maybeck Animal Hospital , general partner of Grant Animal Clinic, and runs the successful veterinary/animal health blogs Web-DVM and Dr. Roger’s Holistic Veterinary Care. Dr. Welton fulfills his passion for lacrosse through his lacrosse and sport blog, The Creator’s Game.

Leptospirosis is a potentially fatal disease caused by the Leptospira bacteria. Leptospira is a cork screw shaped bacteria that effectively self-propels itself in fresh, standing water, such as puddles, ponds, and lakes. The disease is transmitted when dogs and other mammals come into contact with fresh, standing water that is contaminated with the bacteria. Contamination is common given that it occurs via the urine of asymptomatic rodent carriers, most commonly squirrels, rats, and mice.
The Leptospira bacteria attack the canine liver and kidneys leading to failure of each organ system. Once the dog patient is showing clinical signs (vomiting, fever, jaundice, dehydration, shock), even with aggressive in hospital, intensive care treatment, the disease carries a 30% mortality rate. As we continue to clear land for development and encroach into lands that were previously wildlife habitats, the disease continues to rise in incidence.
My motivation for blogging about Leptospirosis is the result of two very concerning areas of misinformation regarding this disease. One is that small companion dogs that spend little time outside and/or dogs that live in suburban or urban environments are not at risk. This could not be further from the truth. Wherever there is water and rodents, there is a risk of Leptospirosis.
In fact, suburban and urban environments actually carry a higher incidence of disease because wherever there are people that create trash and waste, rodents tend to congregate and reproduce. That is why New York City is one of the biggest hot spots of Leptospirosis. We actually see more Leptospirosis in small and toy breed dogs that are popular in suburban and urban environments in comparison to other breeds for these reasons.
The other misinformation that needs clarification comes mostly from breeders that put completely illogical and baseless fear into new dog owners that purchase puppies from them about the “danger” of the Leptospirosis vaccine and warn them not to listen to their veterinarian when he/she recommends Leptospirosis as a core vaccine. Some even go so far as the make the purchasers of one of their puppies sign a contract that they will not allow the vaccine to be administered.
Breeders that make these claims do so with no basis in science and medicine. The vaccine is very safe and the 4 strain Leptospirosis vaccine is very effective in preventing the disease.
If these breeders actually worked in the veterinary medical profession, they would clearly learn how absurd fearing the vaccine more than the disease itself is. They would witness how revoltingly sick dogs present when infected with Leptospirosis and they would see the tragedy of 30% of infected dogs dying from a virtually 100% preventable disease. For the lucky dogs that survive Leptospirosis infection, they would see the financial burden put on the families that had to pay for treatment, since Leptospirosis is a zoonotic disease, that is, a disease potentially transmitted to people; requiring referral to expensive isolation facilities for treatment.
Leptospirosis is now endemic throughout the entire continental United States. As such, it is considered a necessary core vaccine in dogs by the American Veterinary Medical Association, American Animal Hospital Association, The American College of Veterinary Internal Medicine.
Dr. Roger Welton is a practicing veterinarian and highly regarded media personality through a number of topics and platforms. He is the author of The Man In The White Coat: A Veterinarian’s Tail Of Love. In addition to being passionate about integrative veterinary medicine for which he is a globally recognized expert, Dr. Welton was also an accomplished college lacrosse player and remains to this day very involved in the sport. He is president of Maybeck Animal Hospital , general partner of Grant Animal Clinic, and runs the successful veterinary/animal health blogs Web-DVM and Dr. Roger’s Holistic Veterinary Care. Dr. Welton fulfills his passion for lacrosse through his lacrosse and sport blog, The Creator’s Game.
 Since this just happened to me – again – just yesterday, I am about to vent! For those of you that do not enjoy my rants, navigate away now, for I am annoyed!
Since this just happened to me – again – just yesterday, I am about to vent! For those of you that do not enjoy my rants, navigate away now, for I am annoyed!
As an avid runner, I was in the midst of a 5 K run yesterday as I was about to pass a woman with a Miniature Pinscher on a leash walking toward me with her face in her phone texting (or Facebooking, or Snapchatting, etc., etc.). If she had bothered to look up from her phone, she could have seen from half a mile away if she actually cared to restrain her dog from attacking my ankles mid stride as I passed her. Since here eyes were not poised to look up from her phone anytime soon, I actually yelled, “On your left, restrain your dog!” having been there, done that far too many times with clueless people and their little dogs and knew what was to come.
Despite her looking up and seeing me with plenty of time to collect her dog, she did not, and once again, I had a seemingly rabid little dog attacking my ankles as I nearly tripped over the leash as I ran by. As a string of expletives were on the tip of my tongue to hurl that the woman, my self control thankfully won the day and I simply turned around and shot her a look of death. While she did not even bother to apologize, I am hoping that the fact that she could not maintain eye contact with me for more than a nanosecond got enough of the point across that she has learned from this experience and will not let it happen again, I am afraid that I am not optimistic.
Let me be clear that as the former owner of a Yorkie, this is not a rant against little dogs. It is instead a rant against the lazy, ignorant, and discourteous fools that all too often adopt these little dogs without the faintest clue of how to raise them or seek out help to assist them. All they see is a cute little thing that looks like a little stuffed animal that they think will live on their lap and travel in their purse. They have no idea that many of these little dogs ( Terriers, Min Pins, Chihuahuas, etc.) if not properly trained and socialized can be very territorial and have a bad case of “little man syndrome” not unlike that of Scooby Doo’s Nephew, Scrappy Doo.
I can empathize with people who get themselves into situations that they do not understand. I can forgive them for having no clue how to train little dogs and even for failing to seek professional help when they clearly are out of their league. What I CANNOT forgive is the inability to recognize that your dog is going to attack my ankles as I run past him and do nothing to reign in the length of the leash to prevent it, or have your face so cluelessly buried in your phone that you fail to even know that I am approaching (not to mention all of the other surroundings walkers should be aware of for safety’s sake!
That is all. I feel much better!
Dr. Roger Welton is a practicing veterinarian and well regarded media personality throughout a number of subjects and platforms. In addition to being passionate about integrative veterinary medicine for which he is a nationally renowned expert, Dr. Welton was also an accomplished college lacrosse player and remains to this day very involved in the sport. He is president of Maybeck Animal Hospital , runs the successful veterinary/animal health blogs Web-DVM and Dr. Roger’s Holistic Veterinary Care, and fulfills his passion for lacrosse through his lacrosse and sport blog, The Creator’s Game.
 As medical marijuana becomes legal and accessible to more people in more states, pet owners are looking for ways they can use this new family of medications to help their pets. In humans, marijuana and hemp products, and their extracts, are being touted to treat a wide variety of syndromes and diseases. I know individuals who suffered from seizures, or chronic pain, and their lives have dramatically changed for the better, thanks to cannabis-made medications. Fortunately, there are well-designed studies to back up many of these claims…in people.
As medical marijuana becomes legal and accessible to more people in more states, pet owners are looking for ways they can use this new family of medications to help their pets. In humans, marijuana and hemp products, and their extracts, are being touted to treat a wide variety of syndromes and diseases. I know individuals who suffered from seizures, or chronic pain, and their lives have dramatically changed for the better, thanks to cannabis-made medications. Fortunately, there are well-designed studies to back up many of these claims…in people.
When it comes to pets, we aren’t so lucky. Can we extrapolate human data to apply it to dogs and cats? We do with many other drugs quite often, but we must be cautious. Does the law allow for pets to use medical marijuana? The laws are rather silent on pets, making it more risky. Here’s a breakdown.
A quick internet search for legitimate information on cannabis products for pets yields primarily companies selling these products. Obviously, they will tell you their particular product or brand is superior to the others, and their product will treat, manage, or even cure a long list of diseases. We need to wade through the advertising and self-promotion and get down to facts.
CBD, THC, cannabinoids…the basics
Marijuana and hemp are plants in the genus Cannabis. Many different species and strains of these plants exist, and almost 500 different compounds have been isolated from these plants, all with potential medicinal uses. Of these, over 80 are classified as cannabinoids. Different plants contain varying levels of cannabinoids and other compounds.
Every chemical has its own unique properties, and much more research will be needed for us to understand the full potential of this array of potential medications. For our purposes, there are two main cannabinoids that you’ll see mentioned the most: CBD and THC. CBD (cannabidiol) is the “medicine-y” cannabinoid. It’s extracted from a hemp plant, but lacks the psycho-active effects most people think of when they think of marijuana. The molecule responsible for that “high” one can get from marijuana is the other cannabinoid called THC (TetraHydroCannabinol). Think of CBD as the president of the science club, and THC as the party girl, if that helps.
The marijuana plant contains more THC, the chemical responsible for the “high”, while the hemp plant is more fibrous, and contains very little THC. Instead, hemp’s main compound is CBD. What makes us call one plant hemp and the other marijuana if they are both in the same family? Basically, more THC earns it the name “marijuana” while less THC (<0.3% depending on who you read) makes the plant hemp, or even “industrial hemp.”
There are also synthetic cannabinoids out there. The laws are more lax on these, making them “less illegal”, as most of the rules the DEA makes are about the compounds extracted from Cannabis plants (see below). Two of them are actually FDA approved (for human use!) Marinol is prescribed to help AIDS patients not lose their appetites and maintain body weight. Cesamet is prescribed to patients undergoing chemotherapy to help reduce the nausea and vomiting which can happen too commonly. It’s also being used (again, in people) to treat chronic pain and even Irritable Bowel Disease!
While these synthetic cannabinoids sound like a great thing, patients taking them report they don’t seem as effective. Apparently, the synthetics contain one and only one compound, while the extracts contain mainly that compound, but have other cannabinoids along for the ride that seem to have an additive effect. So, bottom line, the products from plants, as of now, seem to work better.
Giving cannabinoids to pets
I know very few veterinarians who recommend these products, for a variety of reasons. Little to no data exists on what dose is safe and/or effective. Little is known about drug interactions. Next to nothing is known about long-term use, simply because the state laws allowing us to conduct large scale clinical trials with it are relatively new. There is absolutely no regulation of production of these products, so we have no way of knowing if what is claimed on the bottle is what actually is in the bottle. Finally, the constant changing of the legal status of these products makes many veterinarians want to keep their noses clean and avoid the whole legal mess until the federal and state laws can come to some agreement.
Here’s a taste of what we do know.
CBD has great promise in the treatment of seizures, but appears to be poorly absorbed into dogs’ bodies when given orally. As far back as 1988, we knew cannabinoids had great potential as a treatment for seizures. Six dogs were given the CBD through an IV, then orally to compare. The IV doses were absorbed into the blood stream and eliminated via the liver. The medication hung around a while too, with a half-life of 9 hours! The oral dosing was not at all absorbed (none detected in the bloodstream) in half the dogs, and the other three that did absorb it had negligible levels. This study was only of six dogs, so we cannot draw any major conclusions from it. Yet, it does not seem promising for CBD’s as an oral option, unless presented in a different version or compound than the one used. Obviously, much more research needs to be done. (Pharmacokinetics of cannabidiol in dogs. Drug Metab Dispos. 1988 May-Jun;16(3):469-72.)
CBD might inhibit the cytochrome P450 enzyme. Here’s the research on it. Not a bad paper, but everything was done in vitro, (where most research starts) and nothing performed in an animal. Chemicals can behave differently than cells in a liver. And what is cytochrome P450 and why do we care? Oh, you care! This is a very important enzyme in the liver that is responsible for metabolizing (breaking down) medications or toxins. If this enzyme is inhibited and your pet is on other medications, it could, theoretically, cause the circulating dose of those other medications to increase, which is not always a good thing.
Dogs may have up to ten times more CB receptors than humans. In order for any chemical to interact with a living organism, there have to be receptors on the cells somewhere in the body. Imagine a catcher’s mitt that has a unique shape that only a certain size and shape of ball can fit into. That is what the cells in our brains, liver, and even skin have. For example, glucose receptors seek out glucose and bind to it. The CB receptors are like catchers mitts sitting on the cells and waiting for a cannabinoid molecule to be caught. When it is, the cell absorbs the molecule, chemical reactions happen, all kinds of magic. Bottom line – the more receptors an animal, or even an organ, has, the more sensitive that animal, or organ, is to that chemical. With dogs having 10 time more receptors for cannabinoids than people, they could potentially be 10 times more sensitive! This must be taken into account for both dosing, and thinking of side effects. (Houghston, SW Vet Symposium 2016)
So, take the first paper into account, where the CBD’s did not seem to enter the bloodstream of dogs when given orally. Now we know dogs have 10 times more CB receptors than people. How the heck do we decide on a dose?
That is precisely the problem.
CBD has been shown to reduce seizures in rats. We’ve also learned, anecdotally, that cannabinoids help epileptic humans as well. We suspect it works by inhibiting the CB receptor, and/or reducing calcium fluxes in neurons. (Izzo AA. Non-psychotropic Plant Cannabinoids: New Therapeutic Opportunities from an Ancient Herb. Cell Press, Elsevier; 2009:515–527.)
CBD may be a potent neuroprotector. Once nerve cells die, they are gone forever. This is why brain damage of any kind, in any species, is such a big bad deal. Izzo et al suggests CBD’s may prevent brain cell death in certain situations, and can even reverse brain damage resulting from lack of oxygen… in rats.
Lesser-known cannabinoids (CBC and CBG) have demonstrated great antimicrobial activity. With all the antibiotic resistant bacteria we have in the world, a new medication that can possibly kill “super-bugs” would be wonderful!
There are many other great studies out there on rodents, giving us hope for future applications. However, it’s a start, and much more needs to be done.
So what is legal, and what isn’t?
And why is this so complicated?
Web-DVM guest blogger Dr. Karen Louis is a practicing small animal veterinarian. See more of her articles at her blog at VetChick.com
 It is time for my yearly pet New Year resolutions that I suggest to all pet owners for the coming year!
It is time for my yearly pet New Year resolutions that I suggest to all pet owners for the coming year!
Walk Your Dog For 20 Minutes Every Evening
Exercise outside in the back yard is great and any dog is lucky to live in a home with a yard where he is free to run and play. But…nothing compares to the walk on the leash outside of the confines of the home that give the dog a sense of freedom and excitement the back yard just does not provide.
The mental and physical benefits of a nice walk cannot be over stated as a routine that provides new sights, smells, and enhances the canine bond with his owner. The adrenaline rush and excitement of the walk is especially beneficial for senior aged dogs to get arthritic joints moving, maintain muscle tone, and stimulate the brain to slow the progression of senility (doggie dementia).
And guess what? It’s good for you too! My 8 year old son and 6 year old daughter are even excited to get in on our almost 11 year old Lab’s nightly after dinner “Energy Walk.” My son even readily abandons his Xbox that he got for Christmas rather than miss the opportunity to stroll around the neighborhood with Bernie, gaze at the stars, and take in the sounds and scents of the evening.
Purchase Pet Insurance
The cost of veterinary care rises on average by 4%-6% per year. This does not occur because veterinarians are greedy, but because the costs of running a veterinary hospital go up by 4% – 6% per year. These costs include reference lab fee increase, regulatory and licensure fee increases,property tax increases, tangible tax increases, inventory cost increases…I could go on here, but you get the point. With this increase in health costs exceeding the rate of inflation by 1.5 to double, do the math and one can see that at some point, the cost of quality veterinary health care can become unsustainable for many pet owners.
It is best to purchase pet insurance BEFORE your pet has experienced any significant health concerns that would be deemed pre-existing conditions that would be excluded from coverage. It is also best to avoid pet insurance companies that are owned by human insurance companies. I have seen many reputable pet insurance companies go to hell in a hand basket after having been bought up by human insurance companies. Obamacare does not apply to pet insurance, so they are free to weasel their way out of paying out claims to their heart’s content.
Stop Falling For Gimmicky Pet Foods And Stick With Trusted, Reputable Brands
Every time I turn my head, there is a new pet food on the market capitalizing on the grain free, corn is the devil, and byproduct ingredients are hair and hooves craze. Some call themselves “holistic” diets, although no standard, classification, or pet food watch dog agency has a criteria or designation for such a claim.
I am amazed by the amounts of money pet owners will spend on unproven diets that are usually not nutritionally well balanced, do not have AAFCO (American Association of Feed Control Officials) certification, and have nothing impressive about them other than a great marketing department.
At the risk of attracting rants from conspiracy theorist trolls that are convinced veterinarians base their opinions on a pet food industry that gives us huge kickbacks and sends us on lavish vacations, I will advise you to stick with the most trusted diets. Why do we trust certain diets? Because of their commitment to species appropriate, breed appropriate nutritional balance, research and development, and quality control.
Royal Canin and Hills year in and year out fulfill all of these criteria and are usually a great deal less costly than whatever new pet food du jour is the flavor of the moment.
Happy New Year everyone! Make 2017 a great one!
Dr. Roger Welton is a practicing veterinarian and well regarded media personality through a number of subjects and platforms. In addition to being passionate about integrative veterinary medicine for which he is a nationally renowned expert, Dr. Welton was also an accomplished college lacrosse player and remains to this day very involved in the sport. He is president of Maybeck Animal Hospital , runs the successful veterinary/animal health blogs Web-DVM and Dr. Roger’s Holistic Veterinary Care, and fulfills his passion for lacrosse through his lacrosse and sport blog, The Creator’s Game.
 I can’t think of a disease that causes more owner anxiety than diabetes. Something about having to give a shot twice a day, every day, to an animal you love is very daunting. Then you do it a couple times and suddenly, it’s a breeze! I’ll try to help you get “breezy” fast!
I can’t think of a disease that causes more owner anxiety than diabetes. Something about having to give a shot twice a day, every day, to an animal you love is very daunting. Then you do it a couple times and suddenly, it’s a breeze! I’ll try to help you get “breezy” fast!
Insulin is kept in the refrigerator. Some pens made for humans can be left out for periods of time, but for the most part, plan on refrigerating the insulin. If you have a decent drive to the pharmacy or vet office, bring a little cooler to bring the insulin home. It needs to be gently mixed before each dose. Vetsulin, an insulin made specifically for dogs and cats, can be shaken like a polaroid picture. Other insulins need to be gently inverted in a rocking motion, not shaken like orange juice.
Your veterinarian will show you how to give shots, and make sure you get some practice with saline solution! Here’s some pointers (hoping to have a video soon!):
If multiple people will be giving the shots, I suggest having a pow wow on measuring the insulin. 3 units to my eyes might look like 3.5 to yours. So, get everyone on the same page.
Pick a time (two times actually, 12 hours apart) and stick with it. Most people do 7 am/7pm or something similar. I have a client who works late and gives the insulin at midnight and noon! Do what works with your schedule. I often feed the animal first, make sure they eat, then give the insulin. Some veterinarians recommend giving the shot 30 minutes before a meal. That makes the most sense biologically, but then what if the pet doesn’t eat? You have insulin in them that you can’t get out! And now we worry about their blood sugar dropping too low. If we make sure they eat before giving the shot, that’s a non-issue.
Here’s how to handle other common questions:
How can you tell if it’s working? How do you know when to worry? coming up are my articles on monitoring and diet as well!
Web-DVM guest blogger Dr. Karen Louis is a practicing small animal veterinarian. See more of her articles at her blog at VetChick.com
As I was at the North American Veterinary Conference getting trained in acupuncture a few weeks ago and seeing first hand its benefits and practical applications, I really began to take a look at our western culture and how generally resistant it is to it and many other alternative treatment modalities. The first question I pondered was, why not explore and offer these treatment modalities as part of an integrative medical approach to patient wellness? In the process of mulling this around in my mind, in the past two weeks, two experiences/realizations made it abundantly clear exactly why our culture has heretofore been overwhelmingly dismissive of alternative medicine.
Before going further, it is first important to compare traditional western medicine with alternative medicine to provide a clear contrast of these different sides of medicine. Western medicine is predicated upon the notion of identifying the disease and treating it directly: a pill here, a surgical procedure there, and the patient gets better…a lot of the time. Alternative medicine is more geared toward boosting the body’s intrinsic ability to heal itself with modalities that include traditional Chinese medical alternatives such as herbal medicine and acupuncture, nutritional and nutraceutical therapy; as well as more high tech alternative options, such as low level laser tissue rehabilitation or electro-acupuncture.
The pros of the western approach is diagnostic capability (x-rays, blood work, ultrasound, blood pressure, etc.), often more immediate results, and the ability to save life through through the application of fluid therapy, pharmacological agents, and hemorrhage control. The main con of this approach is that application of these treatment modalities are frequently fraught with side effects. In the case of chronic disease, long term drug therapy can range from causing side effects that range from mild to severe or even life threatening. Invasive surgery can carry great risks are post-operative adverse effects that may last a lifetime.
The main pro of alternative medicine, is the management of disease without adverse side effects and often the ability to avoid invasive surgery and potentially harmful drug therapy. The main con is the lack of diagnostic capability to provided a concrete diagnosis, and often it lacks real strategies for saving life in times of crisis (acute trauma, hemorrhage, shock, etc.).
So which is better? Which one should we choose for ourselves and for our pets? The answer it each of these questions is, BOTH. The truth is that each branch of medicine has important practical application in treating disease and in the maintenance of wellness. This combination holistic approach is called integrative medicine, meaning that we address the disease, utilizing diagnostics and managing pain, inflammation and life threatening circumstances, but then for the long term look to support the “whole” patient with optimal nutritional considerations and any combination of supplements, herbal therapy, acupuncture, and low level laser therapy. That is what is best for the patient, and that is how everyone should be practicing medicine.
So why is this so often not the case? Why do doctors, instead of practicing integrative medicine, opt instead to draw lines in the sand and refuse to acknowledge that both forms of medicine have their place in maintaining the wellness of a patient? Well, ego probably plays a significant role in this circumstance, but I wish it were that simple.
The truth is, that there are two problems at work here. The first is that we live in a fast paced, results based society that often demands immediate results and wish for a simple injection or pill to make the patient better so that he.she may get on with his/her life. As an example, I have a friend who suffers from Crohn’s Disease, an often debilitating inflammatory disease of the gastrointestinal system. During times when he has taken the initiative to eat a well balanced diet with a lot of unprocessed fruits and vegetables, as well as probiotics (good GI bacteria) to promote good digestion, he has felt better and done better. But…he is a very busy man and is tired when he gets home from work, so rather take the time to prepare healthy meals for each day or even cook at home, he often survives on fast food and vending machine foods for sustenance, and to tolerate it, has to load up on antacid and GI anti-inflammatory pills for days at a time.
The other barrier for consideration of alternative therapy is from my view, the biggest obstacle: insurance companies. In veterinary medicine, we do not have to deal with health insurance companies nearly on the same level as on the human side, but a lot of innovation in veterinary medicine has its roots in human medicine. Pet owners’ expectations in the treatment of their pets also has its roots in their own experience with health care…they are less likely to be open to alternative medical therapy if none are ever offered for their own care. The bottom line is that human health insurance companies will not cover alternative medical therapy, so even in the cases of western trained doctors that see that value in it (there are many more than people realize), they will not offer it, as they are not willing to offer any forms of therapy that their patient’s insurance company will not pay for. I had a conversation with a human medical doctor just last week who is CEO of a company that runs five physical therapy locations in the county I live. When I mentioned to him that I offer low level laser therapy to my patients and asked if he offers it to his, he told me flat out no. He intimated that he is thrilled to see it gaining such momentum in veterinary medicine because the data is there that proves that it works, but he cannot offer it because none of his patients’ insurance plans will cover it, end of story
In my next post/episode, I will discuss practical applications of integrative medicine that I am using in my practice.
Dr. Roger Welton is the President of Maybeck Animal Hospital in West Melbourne, FL and founder/CEO of Web-DVM.net.
